🧬 When the Immune System Overreacts: The 4 Types of Hypersensitivity (I–IV) Explained
- ToothOps

- Dec 18, 2025
- 6 min read
We love the immune system… until it turns a small problem into a big one.
Allergies, autoimmune diseases, serum sickness, contact dermatitis — they look totally different in clinic, but on an exam they all live under one umbrella: hypersensitivity reactions.
In simple terms, hypersensitivity = an exaggerated or misdirected immune response that ends up harming the host.
The good news for your brain (and your PBL notes):There are only four main patterns — Type I, II, III, and IV. Once you understand the logic of each type, the long list of diseases finally stops feeling random.
This ToothOps guide walks you through all 4 types — what they are, how they work, classic examples, and where they matter in dentistry.

1️⃣ The Big Picture: 4 Types on One Page
Before diving into details, anchor the whole map in your head:
Type | Main Weapon | Timing | Where It Acts | Classic Examples |
Type I | IgE + mast cells | Immediate(minutes) | Mucosa, skin, vasculature | Anaphylaxis, allergic asthma, allergic rhinitis, some food allergies |
Type II | IgG or IgM bound to cell surfaces | Hours–1 day | Specific cells or membranes | Goodpasture syndrome, autoimmune hemolytic anemia, immune thrombocytopenia, myasthenia gravis, Graves’ disease |
Type III | Immune complexes(antigen–antibody) floating in serum | 1–2 days | Vessels, kidneys, joints | Serum sickness, Arthus reaction, SLE, some vasculitides, rheumatoid arthritis |
Type IV | T-cells (CD4+ and CD8+) | 2–3 days (delayed) | Skin, lungs, organs | TB skin test, contact dermatitis, granulomas (TB, sarcoid), chronic transplant rejection |
🧠 Memory map:
Types I–III = antibody-driven (humoral)
Type IV = T-cell–driven (cellular)
Keep that hierarchy in mind as we zoom in.
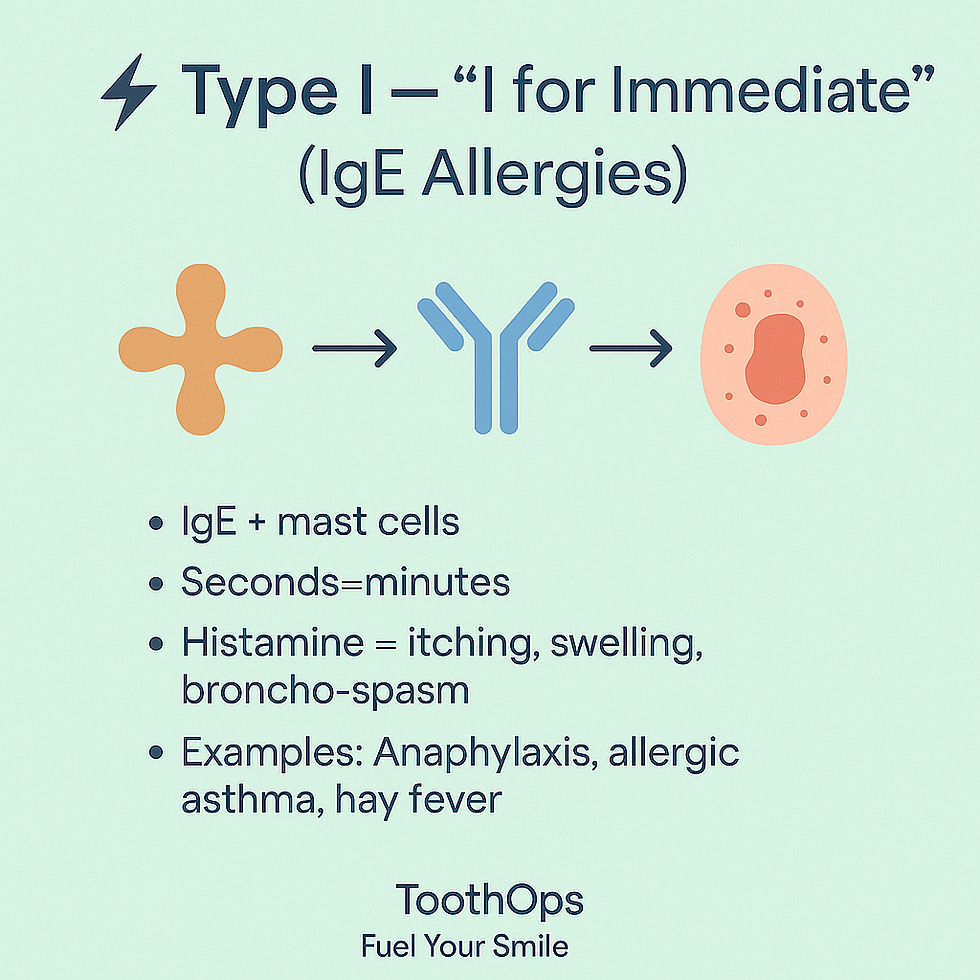
2️⃣ Type I – Immediate Hypersensitivity (“I for Immediate, IgE, Allergy”)
Core idea:Your body makes IgE against an otherwise harmless antigen (pollen, dust mites, foods, insect venom). IgE coats mast cells. On re-exposure, the allergen cross-links IgE on those mast cells → they explode with mediators.
Mechanism in two exposures
First exposure (sensitization):
Allergen enters the body.
Antigen-presenting cells show it to T-cells → Th2 response.
Th2 cells release IL-4/IL-13 → B-cells class switch to IgE.
IgE binds Fc receptors on mast cells and basophils and just… waits.
Second exposure (reaction):
Same allergen returns.
Cross-links IgE on mast cells.
Mast cells degranulate:
Early phase (preformed mediators): histamine, serotonin, eosinophil chemotactic factors
Late phase (newly synthesized): leukotrienes, prostaglandins, platelet-activating factor
Clinical effects:
Bronchoconstriction
Vasodilation and increased vascular permeability → swelling, urticaria
Increased mucus secretion
In severe cases: anaphylactic shock
Classic examples:
Anaphylaxis to foods, drugs, or insect stings
Allergic asthma (extrinsic)
Allergic rhinitis (“hay fever”)
Some acute urticaria reactions
🧠 Analogy Box:Think of mast cells as granule-filled balloons primed with IgE tripwires. The first exposure ties the tripwires on. The second exposure pulls them all at once.
💡 Dental Pro Tip:Always review:
Drug allergies (especially penicillins, local anesthetics).
Latex sensitivity.Have an emergency plan for anaphylaxis (epinephrine, oxygen, airway protocol) — this aligns with ADA and emergency preparedness guidelines.
3️⃣ Type II – “Cy-2-Toxic”: Antibodies Against Cell Surfaces
Core idea:In Type II, antibodies attach directly to cells or extracellular structures and mark them for destruction or interfere with their receptors.
Main antibodies: IgG, IgMMain mechanisms:
Complement-mediated lysis & opsonization
IgG/IgM bind a cell surface antigen.
Classical complement pathway activates → membrane attack complex (MAC) & opsonins.
Result: cell lysis and phagocytosis.
Antibody-dependent cell-mediated cytotoxicity (ADCC)
Antibody-coated cells are killed by NK cells, macrophages, or neutrophils.
Receptor interference
Antibody blocks receptor → loss of function.
Antibody stimulates receptor → overactivity (rare but high yield).
Classic examples to anchor:
Goodpasture syndrome
Antibodies against glomerular and alveolar basement membranes → hematuria + hemoptysis.
Autoimmune hemolytic anemia
Antibodies against RBCs → hemolysis.
Immune thrombocytopenia
Platelets targeted → low platelet count, bleeding.
Myasthenia gravis
Antibodies block acetylcholine receptors at the neuromuscular junction → fatigable weakness.
Graves’ disease
Antibodies stimulate TSH receptors → hyperthyroidism.
🧠 Analogy Box:Type II is like sticking a “target” sticker on a specific cell. The immune system then attacks that tagged cell specifically.
💡 Dental Pro Tip:Patients with Type II processes may present with:
Anemia (fatigue, pallor, tachycardia)
Thrombocytopenia (easy bruising, petechiae)Screen for bleeding risk before extractions or surgeries, and coordinate with the patient’s physician about platelet counts and medication adjustments.

4️⃣ Type III – “3 Is Free”: Immune Complex Disease
Core idea:Antigen–antibody complexes form in the circulation and are not cleared efficiently. They float freely (“3 is free”) until they deposit in tissues, triggering inflammation.
Where complexes land most often:
Blood vessels → vasculitis
Kidneys → immune complex glomerulonephritis
Joints → arthritis
These deposited complexes activate complement → C3a, C5a → neutrophil recruitment → tissue damage.
Classic generalized reactions:
Systemic lupus erythematosus (SLE) – multiple organ immune-complex deposition.
Rheumatoid arthritis (RA) – immune complex-mediated joint inflammation.
Serum sickness
Occurs 1–2 weeks after exposure to foreign proteins/drugs.
Features: fever, rash, arthralgia, lymphadenopathy, proteinuria.
Classic localized reaction:
Arthus reaction
Local, subacute skin reaction at the injection site in a previously sensitized person.
Painful, red, and indurated area hours after vaccination or injection.
🧠 Analogy Box:Think of immune complexes as sticky glitter in the bloodstream. Once it settles in places like vessel walls or glomeruli, the cleanup response causes collateral damage.
💡 Dental Pro Tip:Patients with SLE or RA often:
Take steroids or immunosuppressants (increased infection risk, delayed healing).
Have TMJ or joint involvement affecting comfort in the chair.Gentle technique, shorter appointments, and close communication with their medical team elevate your standard of care.

5️⃣ Type IV – Delayed, T-Cell–Mediated Hypersensitivity
Core idea:Type IV reactions are driven by T-lymphocytes, not antibodies.They are delayed (48–72 hours) because T-cell activation and recruitment take time.
Key players:
CD4+ Th1 cells – secrete cytokines (especially IFN-γ).
CD8+ cytotoxic T-cells – directly kill infected/altered cells.
Macrophages – activated by IFN-γ, participate in granuloma formation.
Two major patterns
Direct cytotoxicity
CD8+ T-cells recognize antigen on cells and kill them.
Delayed-type hypersensitivity (DTH) / granuloma formation
Antigen-presenting cells (macrophages) present antigen to CD4+ T-cells.
Th1 cells secrete IFN-γ → activates macrophages.
If organism is hard to clear (TB, fungi), macrophages and T-cells wall it off → granuloma.
Classic examples:
Tuberculin skin test (PPD)
Induration at 48–72 hours = memory T-cell–mediated response.
Contact dermatitis
Nickel jewelry, poison ivy, some cosmetics or gloves → itchy, eczematous rash exactly where allergen touched the skin.
Granulomatous diseases
TB, histoplasmosis, some fungal infections, sarcoidosis (non-caseating granulomas).
Chronic transplant rejection & graft-versus-host disease
🧠 Analogy Box:Type IV is like a special-operations unit: slower to mobilize, but highly
targeted. If they can’t kill the invader, they build a “prison wall” (granuloma) around it.
💡 Dental Pro Tip:Think Type IV when a patient says:
“I only react days later to that metal or cosmetic.”
“This rash appears exactly where my watch/denture/material touches.”
For dental materials (metals, resins, flavors), consider patch testing via dermatology/allergy and collaborate on alternative materials.

6️⃣
Comparing All 4 Types: High-Yield Exam & Clinic Snapshot
Use this quick checklist when you’re trying to classify a disease:
Is IgE involved? Is it immediate?→ Type I (anaphylaxis, allergic asthma, rhinitis).
Are antibodies binding directly to cell surfaces or receptors?→ Type II (Goodpasture, AIHA, ITP, myasthenia, Graves’).
Are immune complexes floating in serum and depositing in tissues?→ Type III (SLE, RA, serum sickness, Arthus reaction).
Are T-cells and macrophages the main players, delayed by days?→ Type IV (TB test, contact dermatitis, granulomas, chronic rejection).
🧠 Exam Strategy Box:
“Immediate, IgE, allergies, anaphylaxis” → Type I
“Cytotoxic, cell surface, complement, receptors” → Type II
“Immune complexes, vasculitis, nephritis, arthritis” → Type III
“Delayed, T-cells, granulomas, contact dermatitis” → Type IV
a question stem mentions serum sickness, Arthus, or immune complex vasculitis, your brain should instantly flash: Type III.If it mentions PPD, poison ivy, or nickel rash days later, think Type IV.
7️⃣ ToothOps Takeaway: From Memorizing to Understanding
Hypersensitivity doesn’t have to be a wall of memorized lists.
When you understand what weapon the immune system is using and where it’s misfiring, the patterns become logical — and suddenly those PBL cases, NBDE-style questions, and OSCE scenarios feel a lot more manageable.
Small action you can take today:
Pick one disease from each type and explain it out loud to yourself or a friend in two minutes.If you can teach it simply, you own it.
You’re not just memorizing immunology; you’re building the mental framework you’ll use as a future clinician to keep real patients safe.
@ToothOps | Fuel Your Smile 😊
Stay tuned for more insights and educational content in our blog.
Disclaimer: Content is for educational purposes only and not a substitute for medical or dental care.
© 2025 ToothOps | All Rights Reserved



Comments