🦠 Oral Candidiasis Explained: When Chill Candida Turns Chaotic
- ToothOps

- Dec 11, 2025
- 3 min read
Why a normally harmless mouth fungus suddenly acts like it pays no rent.
🧾 TL;DR (30-Second Summary)
Candida normally lives in your mouth — harmless.
It becomes pathogenic when immunity, saliva, or microbiome balance shifts.
The yeast ↔ hyphae dimorphism switch is what makes it invasive.
Biggest risk factors: dry mouth, dentures, antibiotics, immunosuppression.
Treatment fails if the underlying risk factor isn’t fixed (xerostomia, poor denture hygiene, uncontrolled diabetes).
Modern management = topical antifungals + environmental correction.
Candida lives in your mouth 99% of the time like a quiet roommate who minds its business. But the moment your immune system slips?
Boom — it’s free real estate.

This is why you see thrush in infants, denture wearers, diabetics, stressed adults, and immunosuppressed patients. Candida isn’t new — but its behavior changes when the environment changes.
Let’s break down what every dental student, pre-dental, and curious reader should know about this shape-shifting fungus.
1️⃣ What Is Oral Candidiasis? (Simple + Evidence-Based)
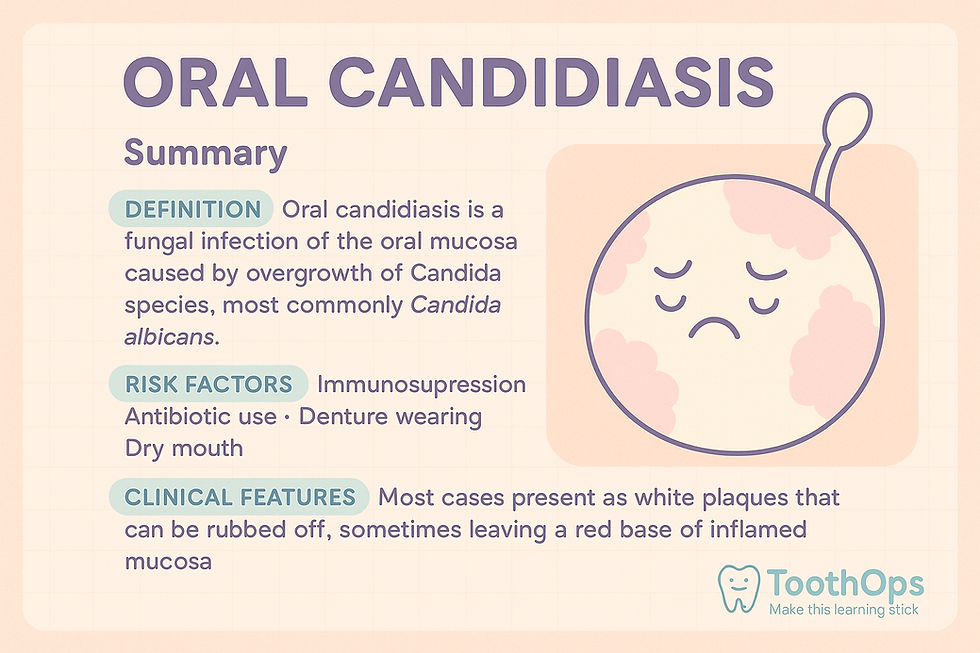
Oral candidiasis is a fungal infection of the oral mucosa caused by overgrowth of Candida species — most commonly Candida albicans.
According to StatPearls (2023) and Neville’s Oral Pathology, Candida is part of the normal oral flora in 30–60% of adults.It only becomes a problem when something disrupts:
mucosal integrity
the immune system,
saliva quantity/quality,
or the microbial balance.
Candida isn’t “new” — it’s opportunistic.
2️⃣ Why Candida Lives in the Mouth (And Usually Behaves)
Candida coexists peacefully with:
saliva (antifungal proteins, IgA)
normal commensal bacteria
intact mucosa
balanced immunity
Think of it like a pet that’s chill as long as the house rules are in place.
But take away saliva…
Introduce chronic stress…
Add a poorly cleaned denture…
Or throw in a course of broad-spectrum antibiotics…
Suddenly the house rules are gone — and Candida becomes feral.
3️⃣ Risk Factors: What Makes Candida Turn Rogue?

Major triggers supported by StatPearls, Burket’s, and Neville Chapter 6:
🔹 Immunosuppression
HIV/AIDS, chemotherapy, systemic steroids, uncontrolled diabetes.
🔹 Xerostomia (Dry Mouth)
Saliva is the mouth’s built-in antifungal system.Low saliva = Candida playground.
🔹 Antibiotic Use
Broad-spectrum antibiotics wipe out protective flora.
🔹 Dentures & Appliances
Biofilms cling tightly to acrylic surfaces — especially if worn overnight.
🔹 Nutritional Deficiencies
Iron, B-vitamins — common in older adults and medically compromised patients.
Your image clearly communicates these in a fun, digestible way.
4️⃣ Candida Dimorphism: The REAL Villain Move

Candida is dimorphic, meaning it can switch forms:
🍇 Yeast Form (Chill Mode)
Ovoid budding cells
Non-invasive
Adapted for survival
Lives peacefully in your mouth
🪵 Hyphal Form (Attack Mode)
Long filamentous structures
Penetrate tissue
Cause inflammation + pain
When immunity dips, Candida flips a biological switch —
and suddenly it isn’t chill anymore…
it’s invading.
Clinically, this explains the burning, ulceration, and bleeding patients feel.
5️⃣ Clinical Presentations (What We Actually See)
Based on StatPearls (2023):
1. Acute Pseudomembranous (Thrush)
White, cottage-cheese plaques → removable.Raw erythema underneath.
2. Erythematous Candidiasis
Red, painful, “burning mouth.”
3. Angular Cheilitis
Cracks and soreness at commissures (Candida + bacteria).
4. Denture Stomatitis
Redness under dentures worn 24/7.Very common.
5. Median Rhomboid Glossitis
Smooth, red, midline tongue patch.
6️⃣ Why Some Cases Don’t Respond to Treatment
Quick preview to tie in your antifungal resistance:
Denture biofilms acting as reservoirs
Poor compliance
Persistent xerostomia
Uncontrolled diabetes
Incorrect antifungal choice
Azole-resistant species
Using chlorhexidine + nystatin together (they inactivate each other!)
This is why antifungal therapy ALWAYS needs environmental correction.

7️⃣ Management: What Actually Works (Evidence-Based)
Supported by StatPearls, Burket’s Oral Medicine, and ADA guidance.
Topical First-Line
Nystatin (swish & swallow)
Clotrimazole troches
Miconazole gel
Topicals work if the cause is also addressed.
Systemic Therapy
Used for severe or refractory cases:
Itraconazole for resistant species
Voriconazole in advanced disease
Fix the Environment (MOST IMPORTANT)
Improve denture hygiene
Remove dentures overnight
Increase salivary flow
Manage diabetes
Reduce smoking
Correct nutritional deficiencies
Fungal infections always return if the environment stays the same.
8️⃣ Mini Story
A patient once told me:“Doc, I thought only babies get thrush!”
Nope. Adults get it all the time — especially if they’re stressed, dry-mouthed, or wearing dentures.
The good news? Once you understand the why, treatment becomes much easier.
💬 Motivational Takeaway
Your mouth is a complex ecosystem — tiny shifts can create big changes. Understanding Candida helps you protect it, treat it early, and keep your smile resilient.
@ToothOps | Fuel Your Smile 😊
Stay tuned for more insights and educational content in our blog.
Disclaimer: Content is for educational purposes only and not a substitute for medical or dental care.
© 2025 ToothOps | All Rights Reserved



Comments