🦠 A.a. vs P.g. | Two Periodontal Pathogens, Two Very Different Disease Stories
- ToothOps

- Jan 1
- 3 min read
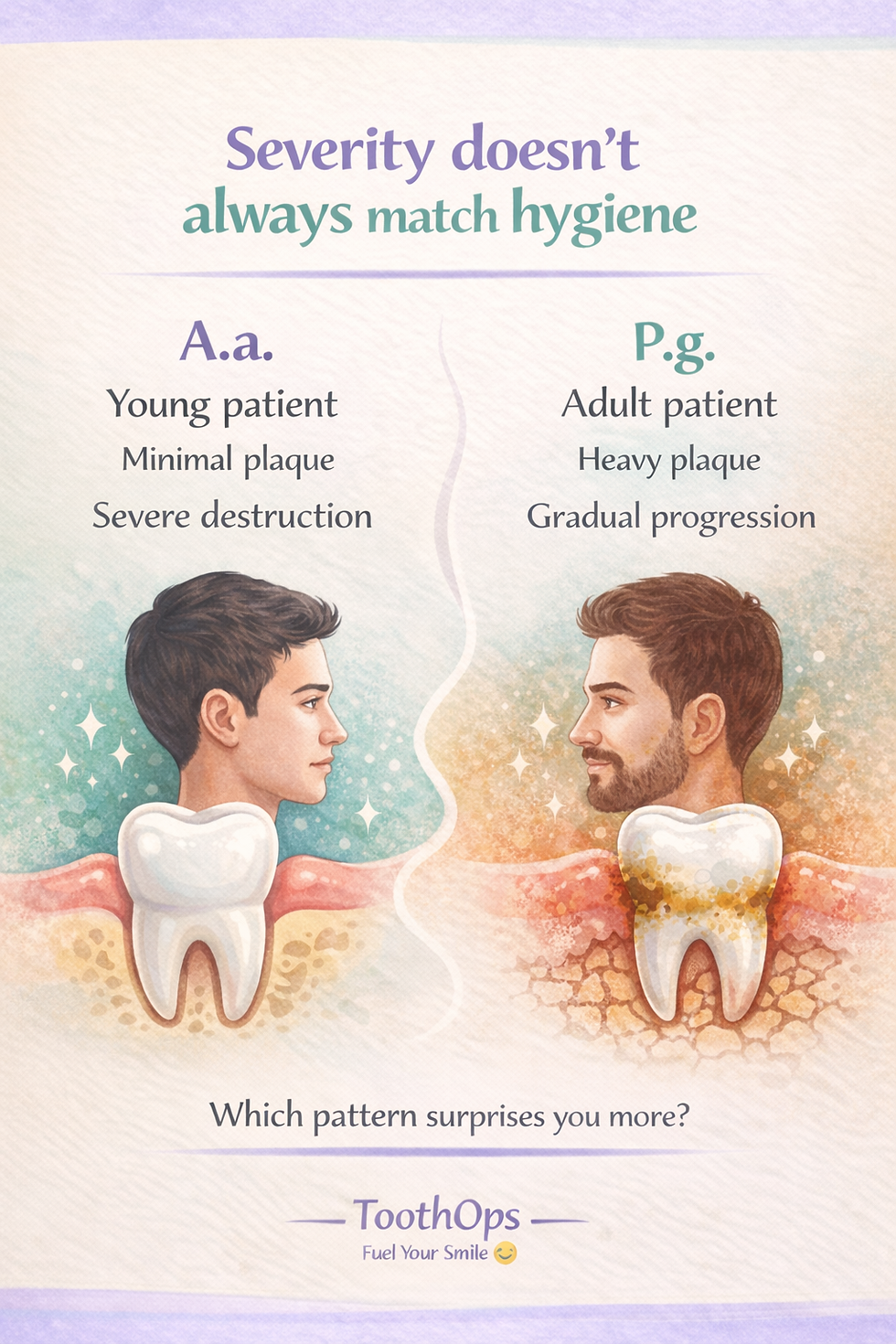
Periodontal disease isn’t one-size-fits-all.
Some patients lose bone shockingly fast with very little plaque.Others progress slowly over decades, despite obvious buildup.
Behind those differences are two key periodontal pathogens every dental student — and informed patient — should understand:
Aggregatibacter actinomycetemcomitans (A.a.)and Porphyromonas gingivalis (P.g.)
They both cause destruction — but they do it in very different ways.

👥 Who This Post Is For (and Why It Matters)
Pre-dental students: Learn how exams test patterns, not just memorization
Dental students: Connect microbiology → radiographs → diagnosis
General readers: Understand why gum disease doesn’t always “look” the same
🧠 TL;DR: If you know how A.a. and P.g. behave, you can recognize disease earlier, explain it better, and treat it more effectively.
1️⃣ Big Picture: Fast vs Slow Destruction
🧠 Analogy Box Think of periodontal disease like fire damage:
A.a. is an explosion — sudden, aggressive, and overwhelming the body’s defenses
P.g. is smoldering smoke — persistent, inflammatory, and quietly destructive over time
Same outcome (bone loss). Very different biology.
2️⃣ Microbiology Basics (High-Yield, No Fluff)
Aggregatibacter actinomycetemcomitans (A.a.)
Gram-negative coccobacillus (short, plump rod-like)
Facultative anaerobe
Highly tissue invasive
Not part of the Red Complex

Porphyromonas gingivalis (P.g.)
Gram-negative anaerobic rod
Strict anaerobe
Black-pigmented colonies on blood agar (heme-dependent)
Core member of the Red Complex (with T. denticola and Tannerella forsythia)
3️⃣ Disease Associations: Who Gets What (and When)
🔥 A.a. → Localized Aggressive Periodontitis (LAP)
(Previously called “juvenile periodontitis”)
Common features:
Teenagers or young adults
Molar–incisor pattern
Vertical/angular bone loss
Minimal plaque, severe destruction
Strong familial clustering
This is why clinicians learn early:👉 Clean mouth does not always mean low risk.
🔥 P.g. → Chronic Periodontitis
Common features:
Adults
Deep periodontal pockets
Heavy plaque and calculus
Horizontal bone loss more common
Polymicrobial infection
P.g. doesn’t act alone — it reshapes the entire microbial community, driving long-term dysbiosis.
4️⃣ Virulence Factors: How Each Pathogen Causes Damage
🔴 A.a. — Leukotoxin (LtxA)
🔥 MOST IMPORTANT
Leukotoxin:
Kills neutrophils and monocytes
Disarms the body’s first line of defense
Allows rapid, uncontrolled tissue destruction
Other virulence factors:
Cytolethal distending toxin (CDT)
Collagenase
Invasive capability
Moderately potent LPS
💡 Why this matters: If immune “first responders” are eliminated, the infection spreads fast — explaining why bone loss can progress rapidly even in young patients.
🔴 P.g. — Gingipains
🔥 MOST IMPORTANT
Gingipains are cysteine proteases that:
Break down collagen → attachment loss
Degrade cytokines → immune evasion
Activate complement → chronic inflammation
Promote bleeding → supports anaerobic growth
Other virulence factors:
Capsule (anti-phagocytic)
Fimbriae (attachment)
Outer membrane vesicles
Highly potent, structurally unique LPS
🧠 Key idea: P.g. doesn’t destroy the immune system — it keeps it stuck in overdrive.

5️⃣ What This Looks Like in Real Life (Clinical Pattern Recognition)
🦷 If you see this… think A.a.:
Teen or young adult
Relatively clean mouth
Isolated deep defects around 1st molars/incisors
Rapid bone loss on radiographs
🦷 If you see this… think P.g.:
Adult patient
Heavy plaque and calculus
Generalized pocketing
Slow, progressive bone loss over years
📌 Exam pearl: Periodontitis is diagnosed by patterns, not just bacteria names.
6️⃣ Common Myths This Comparison Clears Up
🚫 “More plaque always means more disease.”✔ A.a. shows host response matters just as much as biofilm.
🚫 “All periodontitis progresses the same way.”✔ A.a. and P.g. follow completely different timelines.
🚫 “If gums look okay, bone loss isn’t happening.”✔ Aggressive periodontitis can hide clinically.
7️⃣ How Dentists Explain This to Patients (Without Jargon)
Instead of:
“This bacterium produces leukotoxin that disrupts neutrophil chemotaxis…”
Try:
“Some bacteria shut down your body’s first responders, which is why damage can happen quickly even when brushing looks good.”
Clear explanations reduce fear — and build trust.
8️⃣ Fast Master Table (Save for Exams)
Feature | A.a. | P.g. |
Gram stain | Gram-negative coccobacillus | Gram-negative rod |
Oxygen tolerance | Facultative anaerobe | Strict anaerobe |
Disease | Localized aggressive periodontitis | Chronic periodontitis |
Progression | Rapid | Slow–moderate |
Plaque | Minimal | Heavy |
Key virulence | Leukotoxin | Gingipains |
Bone loss | Vertical (molar–incisor) | Horizontal + vertical |
Age group | Young | Adult |
Red Complex | ❌ No | ✔ Yes |
9️⃣ Why This Knowledge Actually Matters
Understanding periodontal pathogens isn’t about memorizing bacteria.
It’s about:
Recognizing when disease doesn’t match plaque levels
Understanding why some patients decline faster
Diagnosing earlier and more accurately
Explaining disease without blame or fear
That’s how science becomes better care.
🌱 Final Takeaway
Periodontal disease isn’t just about hygiene — it’s about biology, immunity, and timing.
When you understand how A.a. and P.g. behave,you stop guessing — and start seeing patterns clearly.
That confidence matters.
@ToothOps | Fuel Your Smile 😊
Stay tuned for more insights and educational content in our blog.
Disclaimer: Content is for educational purposes only and not a substitute for medical or dental care.




Comments